You know that feeling when something feels off at the doctor’s office, but you’re not totally sure if it’s “bad experience” level or “I-need-a-lawyer” level? You’re not alone—and you’re definitely not overreacting. In 2025, patients are more informed, more vocal, and way less willing to let sketchy medical care slide. And that’s a good thing.
This isn’t about hating on doctors. It’s about knowing where the legal line is, so if someone crosses it, you’re not stuck wondering what you could have done. You’ll actually know what to do next.
Below are five insanely shareable, real-world legal rights moves that people dealing with medical issues need in their back pocket right now.
---
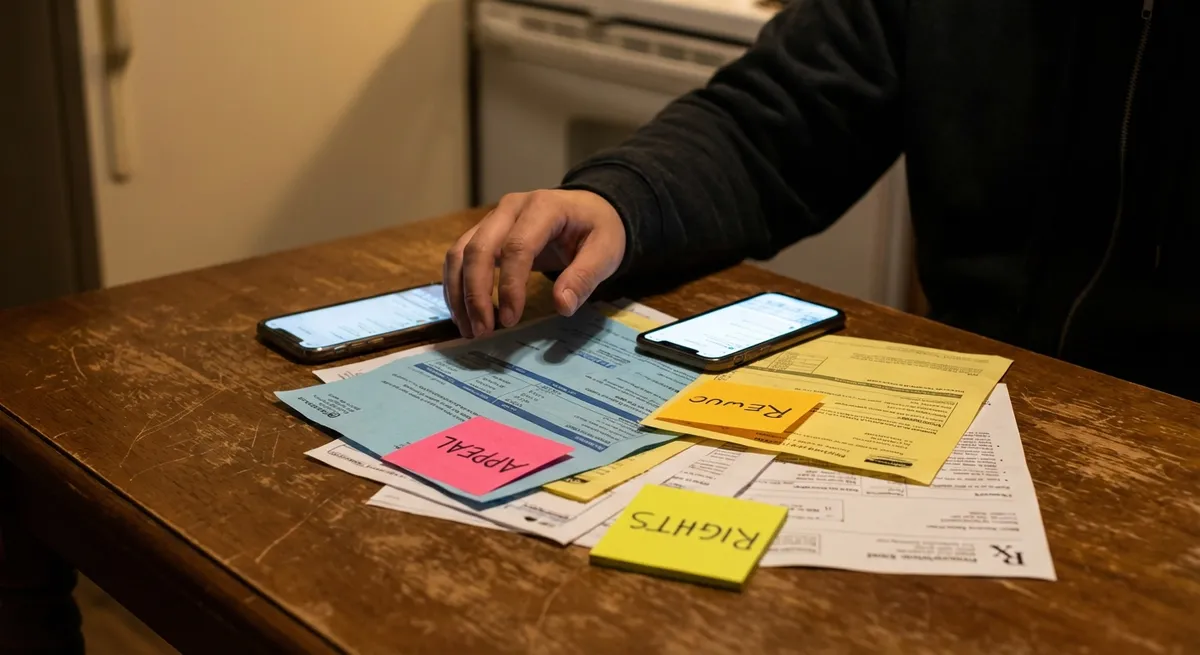
1. Screenshot Everything: Turning “We Never Said That” Into “Yes You Did”
If it’s not documented, it’s easy to deny—and that’s exactly why your receipts matter. When medical care goes sideways, the story often turns into “he said, she said.” But your portal messages, appointment summaries, emails, and even your own notes can become powerful evidence if you ever need to prove what actually happened. This isn’t about being paranoid; it’s about being prepared in a system that doesn’t always remember you as clearly as you remember it.
Start saving copies of test results, visit summaries, and treatment plans the moment you get them. If your doctor says something important in the room—like, “This isn’t serious, you don’t need more tests”—write it down immediately with the date and time, even in your Notes app. If they change their story later, your dated notes can help your attorney see where the breakdown happened. And no, you don’t have to wait for a disaster: organized documentation is like medical insurance for your legal rights. Calm now, clutch later.
---
2. “No, Really—Explain That”: Your Legal Right To Actual Answers
You are not legally required to nod along like everything makes sense when it absolutely doesn’t. In most states, doctors have a duty to get your informed consent—not just your rushed signature on a form you barely read. That means you have the right to know what they want to do, why they want to do it, what the risks are, and what could happen if you say no or choose something else.
If your gut is screaming, “I still don’t get it,” that’s your cue to slow the room down. Say: “I’m not comfortable agreeing yet. Can you explain this in plain language?” If they get annoyed, that’s a red flag—especially if they’re pressuring you to sign or decide quickly. In a malpractice case, unclear or missing informed consent can be a huge deal. Juries look hard at whether you were actually given a real choice. Translation: your confusion today might become a legal turning point tomorrow. Don’t ever apologize for wanting clarity; that’s literally your right.
---
3. The Second Opinion Isn’t Shade—It’s Strategy
Medical culture sometimes treats second opinions like betrayal: “Don’t you trust your doctor?” Legally and practically, that mindset is outdated. You are allowed to question, pause, and get a fresh set of eyes on your case—especially if something feels extreme, rushed, or just plain wrong. Second opinions can catch missed diagnoses, unnecessary surgeries, or dangerous treatment plans before they turn into full-blown harm.
Here’s the part people don’t realize: getting a second opinion can also help your legal case if things later go wrong. If two doctors disagreed, or one suggested a safer path that was ignored, that contrast can be important when lawyers are trying to prove whether the original care met the standard of care. You don’t have to announce it dramatically; just say, “I’m going to think about this and I’d like another opinion before I decide.” If a provider reacts by shaming, rushing, or threatening to drop you as a patient, screenshot that behavior. That’s not just unprofessional—it may matter legally if their pressure leads to a bad outcome.
---
4. When “System Glitch” Becomes Legal Ammunition
We live in the era of portals, algorithms, and auto-populated charts—convenient, until a “system error” delays your test result or buries a critical note. Here’s the catch: when tech fails you in healthcare, it doesn’t magically erase responsibility. Hospitals and clinics are still required to run systems that protect patients, not put them at risk. Blaming “the system” doesn’t always hold up once lawyers start digging into logs and policies.
If you find out something bad happened because a message wasn’t routed, a result wasn’t flagged, or a follow-up never triggered, do not just shrug it off as “one of those things.” Ask direct questions: “When was this result available?” “Who had access to it?” “What is your policy for notifying patients?” Take notes on the answers. If later on you talk to a malpractice attorney, details like this can uncover whether the problem was a random glitch or a pattern of negligence. In a digital world, your legal rights include not being quietly harmed by a broken system someone should have fixed.
---
5. Complaints Aren’t Rude—They’re the First Step To Building a Case
Hospitals and clinics count on most people being too tired, sick, or intimidated to file formal complaints. But when your care feels reckless, dismissive, or dangerous, your complaint can do more than vent your frustration—it can timestamp the problem. A written complaint to the hospital, medical group, or state medical board creates a record that this wasn’t “out of nowhere.” It shows you noticed the issue early and tried to get someone to pay attention.
When you write a complaint, stick to facts over feelings: dates, names, what was said, what was done (or not done), and what happened afterward. Save copies of everything you submit and any responses you get back. If you later bring a malpractice case, those documents can back up your memory and show that the provider or facility was on notice. And no, you don’t need legal representation to start this process—but if your injury is serious, pairing your complaint with an early consult from a malpractice lawyer can turn scattered frustration into a real strategy.
---
Conclusion
Medical mistakes aren’t just horror stories for other people—they’re real, they’re common, and they can be legally actionable when the care crosses the line into negligence. The difference between “I think something bad happened” and “I can actually do something about this” often comes down to what you knew and what you documented in the moment.
Your rights aren’t just pages in a policy binder; they’re tools you can actually use: saving receipts, demanding clear explanations, getting second opinions, questioning system failures, and filing real complaints when the bar drops too low. Share this with the person who always says, “I don’t want to make a fuss at the doctor.” Because in a medical crisis, staying quiet protects the system—not you.
Key Takeaway
The most important thing to remember from this article is that following these steps can lead to great results.