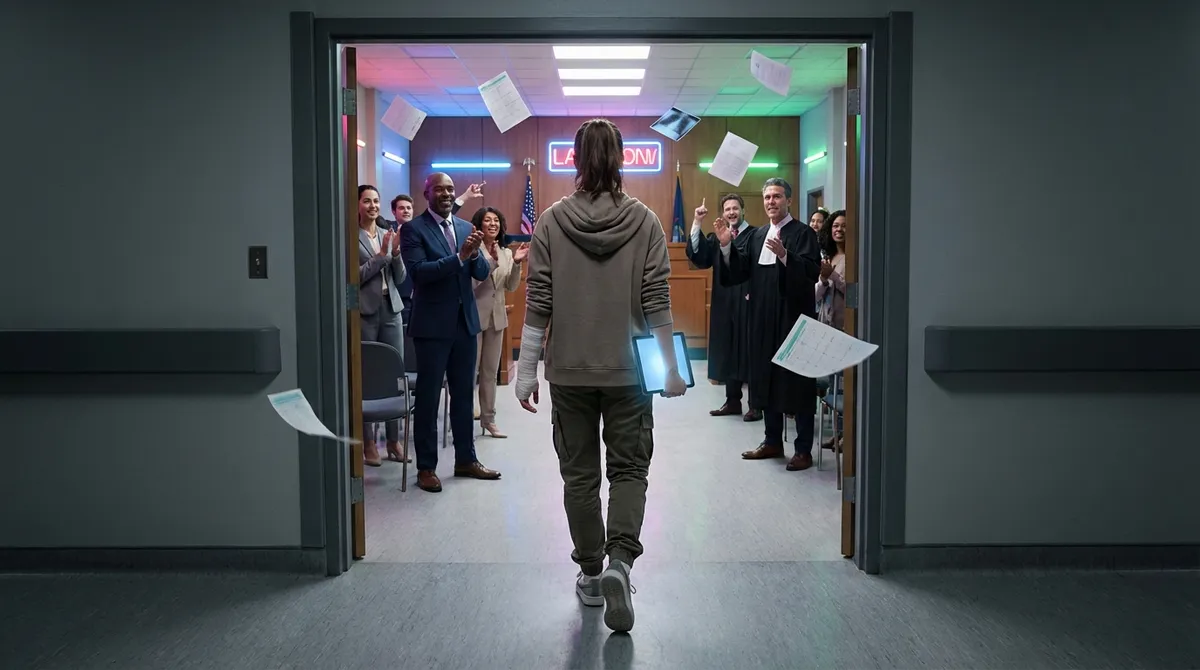
Medical crisis on one side, confusing legal system on the other? That “stuck in the middle” feeling is real. But here’s the plot twist no one tells you: once you understand the legal process, you stop feeling like a pawn and start acting like the main character in your own case. This is your crash course in how a potential medical malpractice claim actually moves—from “Wait, what just happened?” to “Here’s my settlement check, thanks.”
Share this with anyone who’s ever left a hospital thinking, “Something about that wasn’t right.”
---
From “Why Did This Happen?” to “Do I Have a Case?”
The legal process doesn’t start in a courtroom; it starts the moment you suspect something went wrong with your care. That could be a surgery that didn’t fix the issue, a delayed diagnosis, a medication error, or a birth injury that no one fully explains. The law cares about four big ingredients: (1) there was a provider-patient relationship, (2) the provider failed to meet the standard of care, (3) that failure caused harm, and (4) you have actual damages like bills, lost income, or long-term disability.
Here’s where your power move starts: document everything early. Screenshot your MyChart. Save appointment reminders. Ask for the names and roles of everyone involved in your care. The more you treat your medical life like a paper trail, the more clarity you’ll have later. When you go to a medical malpractice attorney—usually for a free consultation—this early evidence can be the difference between “We’re guessing” and “We can actually build this.” You don’t have to show up with a perfect story; you just have to show up with clues.
---
Trending Point #1: The “Receipts or It Didn’t Happen” Era of Medical Records
In med mal, your medical record is not just paperwork—it’s the main character. Every vital sign, lab, medication, and note is a breadcrumb that shows what really happened. You have a legal right under federal law (HIPAA) to access your medical records, usually within 30 days, and providers can’t punish you for asking. This isn’t being “difficult.” It’s being strategic.
The modern glow-up? Patients are treating their health info like a digital bank account. They’re downloading PDFs of records, backing them up in cloud folders, and saving portal messages like chat logs in a lawsuit. If records look altered, incomplete, or missing crucial details, that can become a legal issue too. Lawyers and medical experts later dissect this data to answer the core question: did your care fall below what a reasonably competent provider would have done in the same situation?
Shareable angle: “Normalize asking for your medical records like you ask for your receipts. Same energy, bigger stakes.”
---
Trending Point #2: The Quiet Power of the Expert Witness You’ll Probably Never Meet
You may never sit across from them, but expert witnesses are the unsung drivers of most med mal cases. These are doctors, nurses, or specialists who review your chart and answer the big legal question: was this just a bad outcome, or was it negligence? In many states, your lawyer can’t even file a malpractice lawsuit without an expert’s written opinion or “certificate of merit” saying your case is legit.
This is where your case either levels up or taps out. If experts disagree, things can get intense—and that’s what juries eventually hear about. The defense almost always has their own experts arguing that the care was reasonable or that your injury had another cause. It’s basically a medical debate with legal stakes. You won’t be the one arguing the science, but your legal team will lean on these experts to explain complex medicine in normal language a jury can understand.
Shareable angle: “Your case isn’t just you vs. a hospital. It’s your experts vs. their experts—so picking the right legal team is like picking your all-star roster.”
---
Trending Point #3: The Pre-Lawsuit Maze No One Shows You on TV
TV jumps straight to the courtroom, but real life has a whole hidden chapter before a lawsuit officially drops. Depending on your state, your lawyer may have to send a formal notice to the doctor or hospital that you intend to sue and sometimes wait a specific period before filing. Some states require you to go through pre-suit screening panels or mediation attempts first. These aren’t optional—they’re built into the law.
Behind the scenes, your legal team is doing some heavy lifting: deep-diving your medical records, having experts review your care, mapping out timelines, and calculating your damages (medical costs, lost wages, future care, pain and suffering). During this phase, some cases get quietly settled before a single document hits the court system. Others are dropped if the evidence doesn’t support malpractice. It’s not about how emotional your story is; it’s about how strong the proof is under your state’s laws.
Shareable angle: “Before you ever ‘file a lawsuit,’ there’s a whole level of the game that’s expert reviews, deadlines, and strategy. If no one told you that, you’re not alone.”
---
Trending Point #4: What Actually Happens After a Case Is Filed (Real Talk Version)
Once your lawyer files the complaint, the case officially goes live. The defendant (doctor, hospital, or both) gets served and sends it to their insurance company. Then the real grind begins: discovery. This is where both sides exchange information, take depositions (sworn testimony), and dig into every angle of the story. You might have to answer written questions, provide records, or sit for a deposition where the defense lawyer asks you about your health, your care, and how the injury changed your life.
Most cases don’t ever see a jury. They end in settlement negotiations—sometimes early, sometimes right before trial. Insurance companies weigh risk: how strong is your case, how sympathetic would you look to a jury, and how bad would it be for them if they lose publicly? Your lawyer’s job is to push for max value without promising a fantasy number that isn’t realistic under your state’s caps or guidelines. If you do go to trial, expect a marathon: jury selection, opening statements, expert testimony, cross-examination, closing arguments, and then… waiting.
Shareable angle: “The legal process is less ‘dramatic courtroom monologue’ and more ‘months of organized receipts and chess moves.’ That’s the reality nobody glamorizes.”
---
Trending Point #5: Settlements, Payouts, and What “Winning” Actually Looks Like
“Did you win?” sounds simple. In med mal, it’s not. Winning might mean a settlement that covers your past and future medical care, replaces lost income, and compensates you for pain, suffering, or permanent disability. It can also mean structured payments over time instead of one lump sum, especially if a child or severely injured person needs lifelong care. Your lawyer’s contingency fee (often around 33–40%) plus case expenses come out of whatever you recover, not from your pocket upfront.
There’s also the emotional side. For some people, seeing accountability—a policy change, a training shift, or a provider finally admitting harm—matters as much as money. For others, the process is about securing financial stability after their life was derailed. And here’s the twist: even “strong” cases can lose at trial, and even “tough” cases can settle well. The system is human, imperfect, and sometimes unfair—but understanding how outcomes actually work gives you more realistic expectations and less shock at the end.
Shareable angle: “In med mal, ‘winning’ isn’t just a verdict. It’s getting your life funded, your story heard, and your future back under your control.”
---
Conclusion
The medical malpractice legal process isn’t designed to be user-friendly, but that doesn’t mean you have to wander through it blind. When you know that records are power, experts are key, pre-suit steps matter, discovery is where stories get tested, and “winning” has layers, you stop feeling like the system is happening to you. Instead, you’re an informed player making sharp moves in a complicated game.
If your care went off the rails and something in your gut still says, “This wasn’t just bad luck,” talking to a qualified medical malpractice attorney isn’t overreacting—it’s protecting your future. Screenshot this, save it, send it to the group chat. Information like this doesn’t just go viral—it gives people their power back.
---
Sources
- [U.S. Department of Health & Human Services – Individuals’ Right under HIPAA to Access their Health Information](https://www.hhs.gov/hipaa/for-professionals/privacy/guidance/access/index.html) – Explains your legal right to get copies of your medical records and how providers must respond
- [American Bar Association – Medical Malpractice Overview](https://www.americanbar.org/groups/public_education/resources/law_issues_for_consumers/medmal/) – Breaks down what medical malpractice is and how these cases typically work
- [Nolo – Medical Malpractice: What Is It?](https://www.nolo.com/legal-encyclopedia/medical-malpractice-basics-29829.html) – Consumer-focused explanation of negligence, damages, and how med mal claims move through the system
- [National Library of Medicine (NIH) – Expert Witnesses in Medical Malpractice](https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3370283/) – Discusses the critical role of expert witnesses in evaluating and proving malpractice claims
- [Cornell Law School Legal Information Institute – Statute of Limitations](https://www.law.cornell.edu/wex/statute_of_limitations) – General overview of time limits for filing lawsuits, including medical malpractice in many states
Key Takeaway
The most important thing to remember from this article is that this information can change how you think about Legal Process.