Healthcare doesn’t have to feel like a mystery game where everyone has the rule book except you. When something goes wrong with medical care, most people assume they’re stuck with bad luck, confusing paperwork, and awkward “guess we’ll never know” conversations. Reality check: you have legal rights, leverage, and options—and they’re a lot stronger than you’ve been led to believe.
This is your no-fluff, seriously-shareable breakdown of patient legal rights that actually move the needle when things get messy. Send this to your group chat, your family chat, and that one friend who always says “I don’t want to bother the doctor.”
---
Your Medical Records Are Not a Favor – They’re Your Legal Right
Let’s start with the most slept-on power move: your chart is yours. Not a bonus. Not a “maybe.” A legal right.
Under federal law (HIPAA), you’re allowed to see, download, and get copies of your medical records. That includes doctor notes, test results, imaging reports, discharge summaries, and more. Providers can charge a reasonable fee in some cases, but they can’t just say “no” because they’re busy, annoyed, or worried you’ll ask questions.
Why this matters when things go wrong:
- Your records are often the *first* place med mal lawyers look to see if something was off.
- Missing, altered, or delayed notes can be a huge red flag.
- The timeline in your chart can make or break a malpractice case.
- You don’t need a lawyer to request them—you can start that process today.
What to do in real life:
- Ask for your records **in writing** (patient portal, email, or form).
- Be specific: “All records from [date] to [date], including doctor notes, imaging, lab results, and medication lists.”
- If they stall or delay beyond the legally allowed time (usually 30 days in the U.S.), that’s not just rude—it can be a violation of your rights and a signal to talk to a lawyer.
Hot take: Any provider who makes it weird when you ask for your own records is telling you exactly why you should.
---
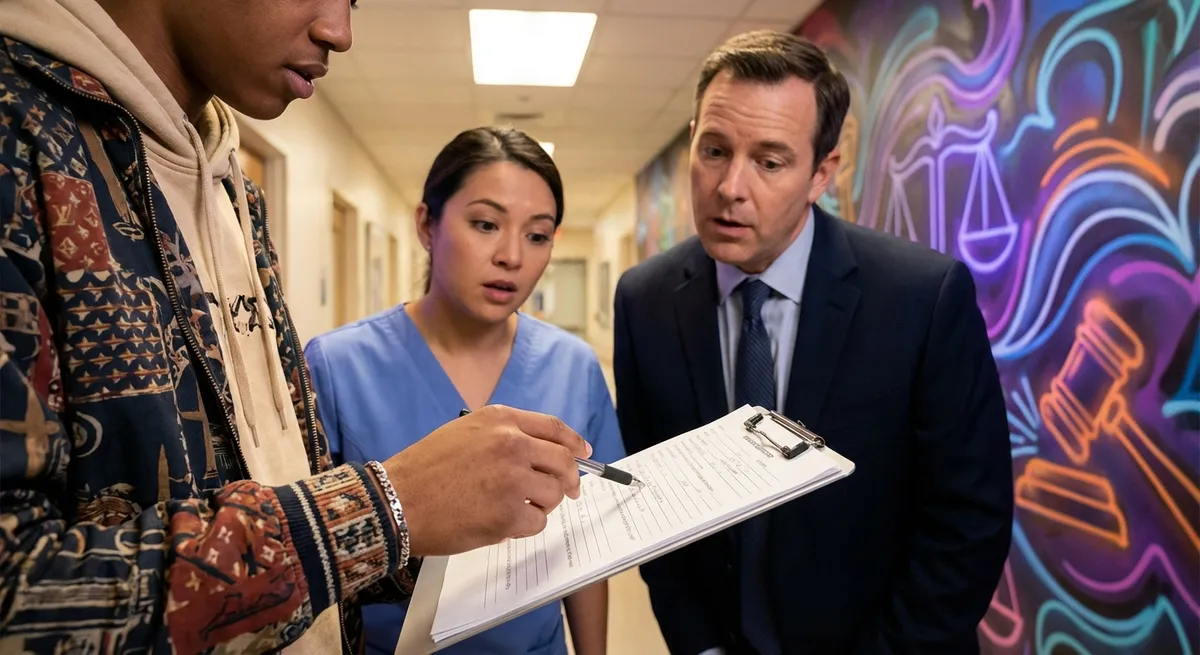
“Informed Consent” Is More Than a Signature You Don’t Read
That clipboard you signed five minutes before a procedure? It’s not just paperwork; it’s a legal battleground.
Informed consent means:
- You’re told what the doctor plans to do
- You’re told the **real** risks, not just the fluffy version
- You’re told the alternatives (including doing nothing)
- You get a chance to ask questions and actually understand the answers
If you weren’t warned about major, known risks or were pressured, rushed, or straight-up misled, that consent form is not the shield they think it is.
Why this is share-worthy:
- A lot of malpractice cases hinge on whether the patient would have said “no” if they had known the full story.
- “You signed a form” does **not** automatically mean you waived your rights.
- Consent isn’t just a piece of paper; it’s a conversation. If that convo never happened, that’s a legal issue.
What you’re legally allowed to do:
- Ask for your signed consent forms after a procedure—yes, you can, and yes, you should.
- Ask, “What are the most serious risks, even if they’re rare?” and “What happens if we wait or don’t do this?”
- If you were never told about a risk that later hits you hard, that’s exactly the kind of detail malpractice attorneys want to hear about.
Bottom line: Your signature is not a gag order. If you were kept in the dark, the law is often on your side.
---
You Can Get a Second Opinion – Without Being “Difficult”
There’s an unspoken rule a lot of patients feel: don’t question your doctor or you’ll be labeled “difficult.” That mindset is pure gold—for hospitals, not for you.
Legally and ethically, you’re allowed to:
- Get a second (or third) opinion
- Transfer your care to another doctor or hospital
- Ask your doctor to share your records with another provider
- Say “I want to think about this before deciding”
Why this matters when care goes sideways:
- A fresh set of eyes can catch mistakes: misdiagnoses, wrong meds, missed labs, or surgery that never should have happened.
- Another doctor can sometimes document concerns in your record—this can later support a malpractice claim.
- If a provider gets defensive or refuses to help you transfer care, that behavior itself can be evidence of a problem.
Real-world moves that protect you:
- Use language like: “I’d like another medical opinion before we move forward. Please send my complete records to [Doctor/Facility].”
- If they drag their feet, document it: dates, times, names, and what they said. Screenshot portal messages, keep emails.
- If a doctor “discourages” a second opinion, that’s not confidence—it’s a red flag.
Here’s the plot twist: empowered patients aren’t annoying; they’re the ones most likely to avoid catastrophic outcomes.
---
You Have a Legal Clock Ticking (Even If You Don’t Feel Ready)
One of the most brutal realities of medical malpractice: your legal rights come with an expiration date.
Every state has a statute of limitations—a deadline by which you must file a lawsuit. Miss it, and it usually doesn’t matter how strong your case is; you might be legally blocked from bringing it.
Complications:
- In some states, the clock starts when the malpractice *happens*.
- In others, it starts when you *discover* (or reasonably should have discovered) the harm.
- There are often special rules for children, government hospitals, or specific types of claims.
- Some states require a “notice of claim” or expert review *before* you can sue—those have their own deadlines.
Why you should not “wait and see” too long:
- Hospitals and insurers are absolutely watching the calendar.
- Evidence can disappear or get harder to track over time.
- Witness memories fade, providers move, and records can become suspiciously incomplete.
What to actually do:
- The minute you suspect something’s off—like a delayed diagnosis, a surgery disaster, or a medication error—start a personal timeline: dates, symptoms, visits, names.
- Use that timeline when you talk to a malpractice attorney. Many offer free consultations.
- Ask directly: “What is my deadline to act in this state?” and “Are there any special notice requirements?”
Your feelings might need time to process; your legal rights do not. The law runs on calendars, not emotions.
---
You’re Allowed to Ask for Help: Lawyers, Advocates, and Complaints Aren’t “Overreacting”
The system often trains patients to be grateful, quiet, and confused. Legally, you don’t have to play that role.
You have the right to:
- Talk to a medical malpractice attorney, even if you’re not sure you “have a case”
- File complaints with hospital patient relations or risk management
- Report serious safety issues to state medical boards or health departments
- Bring someone with you to appointments as a witness and support
Why this is more powerful than people realize:
- A single complaint doesn’t always change the world—but multiple complaints about the same provider can trigger investigations.
- Medical boards can discipline doctors, restrict licenses, or require more training.
- Attorneys can help you access expert opinions, decode records, and figure out whether what happened was a known complication or negligent care.
- Even if you never go to court, asserting your rights can lead to policy changes, better communication, or settlements.
Signals it’s time to stop “being nice” and start taking action:
- You keep getting different stories from the same provider.
- Nobody will give you a clear explanation of what went wrong.
- You’re being pressured to sign something fast (like a release or waiver) after a bad outcome.
- Your gut says, “This isn’t just bad luck.”
You’re not being dramatic. You’re using the tools the law expects you to use when the system fails you.
---
Conclusion
You don’t need a law degree to use your legal rights; you just need to stop believing you’re powerless in a system that depends on your silence.
- Your records are yours.
- Consent is a conversation, not just a form.
- Second opinions are normal, not offensive.
- There’s a legal clock—whether anyone tells you about it or not.
- Reaching out for legal and regulatory help is exactly what those systems exist for.
If something about your care feels wrong, you’re allowed to say it, document it, question it, and act on it. That’s not picking a fight—that’s protecting your future.
Share this with anyone who’s ever said, “I don’t want to make a fuss.” Their health—and their legal rights—are absolutely worth the “fuss.”
---
Sources
- [U.S. Department of Health & Human Services – Individuals’ Right under HIPAA to Access Health Information](https://www.hhs.gov/hipaa/for-professionals/privacy/guidance/access/index.html) – Explains your legal right to access and obtain copies of your medical records.
- [American Medical Association – Informed Consent](https://www.ama-assn.org/delivering-care/ethics/informed-consent) – Outlines ethical and legal standards for informed consent in medical care.
- [MedlinePlus – Medical Records](https://medlineplus.gov/medicalrecords.html) – Consumer-friendly overview of how to get and use your medical records.
- [National Conference of State Legislatures – Medical Liability/Malpractice Statutes of Limitation](https://www.ncsl.org/health/medical-liability-malpractice-statutes-of-limitation) – Summarizes how malpractice time limits vary across U.S. states.
- [Federation of State Medical Boards – Contact a State Medical Board](https://www.fsmb.org/contact-a-state-medical-board/) – Directory for reporting concerns or filing complaints about physicians with state regulators.
Key Takeaway
The most important thing to remember from this article is that this information can change how you think about Legal Rights.