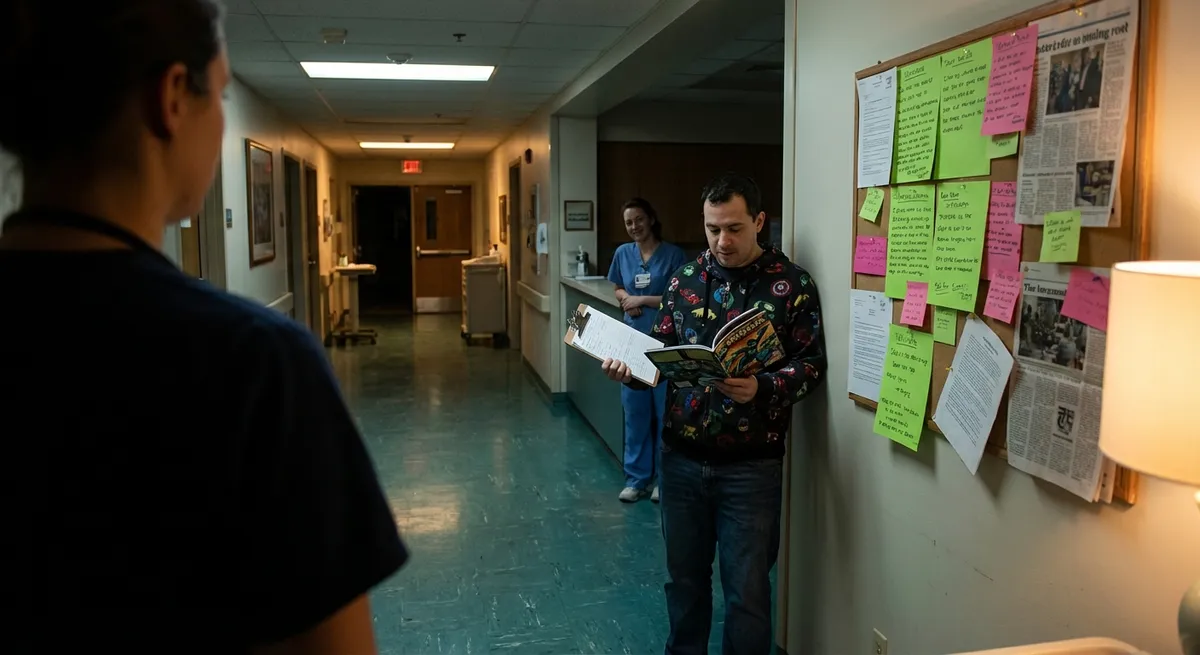
Healthcare drama doesn’t just live on TV. Real patients are out here turning “something feels off” moments into full-on plot twists, paper trails, and court wins. These case study vibes? They’re the receipts showing exactly how tiny decisions (and screenshots) can change the whole storyline.
Welcome to the behind-the-scenes of real medical malpractice energy—where ordinary patients quietly collect proof, ask sharp questions, and sometimes walk out with life-changing legal outcomes.
When “It’s Probably Nothing” Was Actually Everything
In one widely discussed malpractice case, a young woman showed up to the ER with classic stroke symptoms: facial droop, slurred speech, and sudden weakness. The first doctor dismissed her as “too young” and blamed anxiety.
Her partner, who had been tracking her symptoms on their phone, pushed back and insisted everything be documented in her chart—time of onset, what she said, how she was walking. Those timestamps later became critical.
A second clinician finally ordered the right imaging, confirming a stroke. Treatment came—late—but still in time to help. The delay, though, meant permanent deficits.
When the lawsuit landed, the combo of:
- Time-stamped symptom notes
- Discharge paperwork
- Imaging report timelines
created a paper trail no one could ignore. The case settled, and her partner’s “annoying” insistence on documentation turned into the legal backbone of her claim.
Shareable takeaway: Document your symptoms like you’re live-tweeting your own medical story (for yourself, not the internet). Times, changes, what you told them, what they said back—this is the stuff malpractice cases are built on.
Screenshot Energy: How a Patient Portal Note Flipped the Whole Case
A middle-aged man went in for routine surgery and woke up in far more pain than expected. He kept telling staff something felt wrong. Nurses reassured him; the surgeon brushed it off as “normal recovery.”
Days later, his condition tanked. An internal organ had been nicked during surgery, causing a serious infection. The hospital claimed they acted fast and “within standard of care.”
Then his daughter opened his patient portal.
Buried in the notes: a nurse had charted concerns about his vitals and escalating pain hours before anything was done. There were also orders that weren’t followed in time. That quiet digital breadcrumb trail completely undercut the “we moved quickly” narrative.
Those portal screenshots?
- Showed *when* concerns were documented
- Revealed delays between orders and actual care
- Captured discrepancies between what was said vs. what was written
The family’s legal team used the portal data to argue the hospital knew more, and sooner, than they claimed. The case ultimately resolved in the patient’s favor.
Shareable takeaway: Patient portal = your real-time receipts. Read the notes. Screenshot anything that feels off. Future-you (or your lawyer) will thank present-you.
The “Second Opinion” That Exposed a Years-Long Missed Diagnosis
A woman spent years being told her chronic pain was stress, hormones, or “just getting older.” She bounced from provider to provider, collecting vague diagnoses and short-term fixes.
One day, a new doctor ordered imaging her prior clinicians had skipped. The scan showed advanced cancer—something that could have been caught far earlier if standard guidelines had been followed.
The breadcrumb trail:
- Multiple visits with almost identical complaints
- No documented rationale for **not** ordering basic tests
- Guidelines clearly recommending earlier screening based on age + symptoms
Her case turned into a serious malpractice claim, not because cancer happened, but because warning signs were repeatedly downplayed while the standard of care was ignored.
The second-opinion doctor’s records—and the contrast between what should have been done vs. what actually happened—made all the difference.
Shareable takeaway: Second opinions aren’t “being difficult.” They’re quality control. When your story stays the same but the doctor’s plan doesn’t level up, it might be time to switch rooms and reset the storyline.
Family Group Chat Pressure: How Loved Ones Became Key Witnesses
In another major malpractice case, an older patient developed strange confusion and weakness after being prescribed a new medication. Staff brushed it off as “normal aging” and “a little dehydration.”
His family didn’t buy it—and they had proof.
The group chat was full of:
- Videos of him walking and talking normally *before* the new med
- Time-stamped messages describing “he suddenly can’t stand on his own”
- Notes about exactly which medication had just been started
When he later suffered a preventable complication related to that drug, the family’s timeline became powerful evidence. Their real-life digital receipts painted a sharper picture than anyone’s memory could.
In court, those videos and messages were used to show:
- How quickly his condition changed
- How different he’d been before the prescription
- That the family repeatedly raised concerns
Shareable takeaway: Those “should I record this?” moments with your loved one in the hospital? Often worth it. Short clips, quick notes in the group chat—this is modern-day witness testimony in your pocket.
The “Small Detail” Discharge Instruction That Changed Everything
One case turned on something most people toss: discharge paperwork.
A patient with chest pain was sent home from the ER after a quick workup. The doctor verbally said it was “probably muscle strain.” But the discharge instructions, written in template fashion, listed “return immediately for worsening pain, shortness of breath, or new symptoms.”
He returned hours later in full-blown heart attack.
The hospital initially claimed the first visit was appropriate. But the written discharge instructions acknowledged the risk in a way the verbal reassurance did not. That mismatch became central:
- The paperwork quietly admitted “this might be serious”
- The actual evaluation didn’t line up with that level of risk
- The follow-up heart attack made those instructions look like foreshadowing
In the malpractice claim, the discharge note helped prove they knew enough to warn him—but not enough to fully protect him.
Shareable takeaway: Never just toss your discharge papers. Photograph them. Read the fine print. Sometimes the most important legal sentence is hiding in bullet point #4 of the “when to come back” section.
Conclusion
These real-world case vibes all have the same core theme: patients and families weren’t being paranoid—they were paying attention. And that attention turned into power once things went sideways.
Not every bad outcome is malpractice. Not every case wins. But over and over, the same patterns show up in the files lawyers actually take seriously:
- Symptom timelines, written down
- Patient portal notes and messages
- Second opinions that expose the gap
- Family videos, texts, and DMs as quiet witnesses
- Discharge paperwork that says more than the conversation did
You don’t have to be a lawyer to move like someone who understands how medical stories are documented—and later, investigated. Start acting like your health is a high-stakes storyline where everything counts: the questions you ask, the notes you keep, the records you read.
Because if your care ever does cross the line into malpractice, these little “just in case” moves are exactly what can turn your experience into a case study that actually makes the system pay attention.
Sources
- [U.S. National Library of Medicine – Medical Malpractice Overview](https://medlineplus.gov/ency/article/001935.htm) - Plain-language explanation of what medical malpractice is and how it’s defined
- [American Bar Association – Basics of Medical Malpractice](https://www.americanbar.org/groups/public_education/resources/law_issues_for_consumers/medmal/) - Consumer-focused breakdown of how malpractice cases work and what evidence matters
- [Agency for Healthcare Research and Quality (AHRQ) – Patient Safety Primer](https://psnet.ahrq.gov/primer/patient-safety-101) - Background on medical errors, safety culture, and why documentation and communication are so important
- [Cleveland Clinic – Getting a Second Opinion](https://health.clevelandclinic.org/why-you-should-get-a-second-opinion) - Explains why second opinions can change diagnoses and treatment paths
- [Mayo Clinic – Understanding Your Patient Portal](https://www.mayoclinic.org/tests-procedures/patient-online-services/about/pac-20385273) - Overview of patient portals and how to use them to access notes, labs, and visit summaries
Key Takeaway
The most important thing to remember from this article is that this information can change how you think about Case Studies.