When your health gets messy, your legal rights should not. Think of this as your “patient power pack” you wish came standard with every hospital wristband. These aren’t dusty legal rules no one uses—these are real-life, shareable moves people are using right now to push back, get answers, and protect themselves when medical care goes sideways.
Bookmark this, send it to your group chat, drop it in the family text. These are the rights that turn “I feel ignored” into “Here’s what the law says.”
---
Why Legal Rights Matter Before Anything Goes Wrong
Most people only start Googling “patient rights” after something already feels off—pain not taken seriously, test results disappearing, doctors not listening, bills exploding. By then, you’re stressed, emotional, and trying to translate medical jargon and legal jargon at the same time. Brutal combo.
Knowing your rights before a crisis gives you leverage in the moment:
- You stop accepting “that’s just how it is” as an answer.
- You ask sharper questions and demand clear explanations.
- You document better, earlier, and more consistently.
- You can tell the difference between an honest complication and a potential medical error.
- You know when it’s time to call a lawyer instead of hoping it “works out.”
This isn’t about picking fights with doctors. It’s about making sure you don’t get steamrolled in a system that’s busy, understaffed, and not always built around transparency. Your rights exist whether you know them or not—but knowing them turns them into actual power.
Below are 5 trending, screenshot-worthy rights that patients dealing with medical issues are sharing, quoting, and using as receipts when something feels off.
---
1. The “Show Me the Chart” Right: Full Access to Your Medical Records
The old days of mysterious paper charts kept behind the nurses’ station? Over. In the U.S., you have a legal right to see and get copies of your medical records under HIPAA (and similar laws in many other countries).
What this means for you:
- You can request your records—including doctor notes, lab results, imaging reports, and discharge summaries.
- You don’t need a “good reason.” Want them because you’re curious? That’s enough.
- In most cases, they have *deadlines* to respond (often 30 days in the U.S.).
- You can usually get them electronically (PDFs, secure portals, etc.).
- You can ask for corrections if something in your record is wrong or incomplete.
Why this is a power move in potential med mal situations:
- **You see the timeline**: who ordered what, when, and why.
- **You spot contradictions** between what you were told and what was written.
- **You catch missing info** that might matter later (like symptoms you reported).
- If a lawyer ever gets involved, **you’re not starting from zero**—you already have a paper trail.
Shareable script you can actually say or email:
> “Hi, I’d like a complete copy of my medical record for my own use, including provider notes and test results. Please let me know the process and any standard fees. I’d prefer an electronic copy if possible.”
That’s not “being difficult.” That’s you exercising a legal right.
---
2. The “I Need This in Plain English” Right: Informed Consent That Actually Informs
Signing a stack of forms while wearing a hospital gown doesn’t equal informed consent. Legally, consent isn’t just your signature—it's your understanding.
Informed consent means you should be told, in a way you can understand:
- What the procedure or treatment is
- Why it’s being recommended
- What the realistic risks are (not just “low risk”)
- What the alternatives are—including doing nothing
- What could happen if you say no
If they’re rushing or vague, that’s not just annoying—it may be a legal problem.
How to use this right in real life:
- Say: **“Can you walk me through the risks and benefits in simple terms?”**
- Ask: **“What else could we do instead? What happens if I wait or don’t do this?”**
- If you don’t understand, say exactly that: **“I’m not clear enough to feel safe signing this yet.”**
When med mal claims happen, lawyers often zoom in on this exact point: Were you really informed, or were you just rushed through paperwork? Making sure you get real answers now not only protects you medically—it also creates a record that you were actively asking questions.
---
3. The “Pause the Room” Right: Second Opinions Without the Guilt Trip
If a treatment plan feels extreme, confusing, or just off, you can get a second opinion. That’s not disloyal. That’s smart risk management with your own body.
What the law and most ethical codes support:
- You can ask for a second opinion—even within the same hospital system.
- You can request copies of your tests and bring them to another doctor.
- You are not obligated to stay with a provider you don’t trust.
- Insurance often covers second opinions for major procedures (read the fine print).
In med mal land, rushed, one-track decisions can be where serious mistakes happen—wrong diagnosis, unnecessary surgery, missed red flags. A second opinion is like a legal and medical safety check.
How to say it without drama:
> “This is a big decision for me. I’d like to get a second opinion before moving forward. Can you send my records and imaging to [Doctor/Clinic]?”
If they get defensive or try to shame you? That’s not a good sign. And yes, that behavior itself can become part of the story if things later go wrong.
---
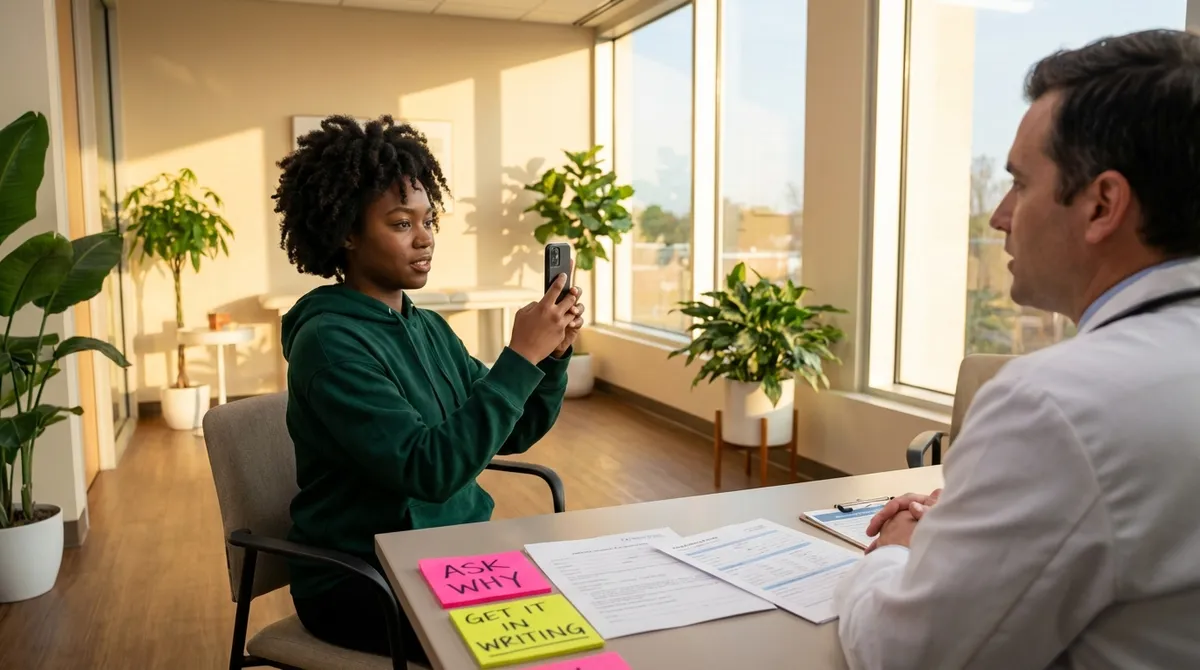
4. The “Receipts or It Didn’t Happen” Right: Documenting Your Care Like a Pro
You have an underrated legal superpower: your own documentation. Courts, regulators, and lawyers love timelines. Confused, emotional memories? Not so much. So you build your own receipts as you go.
How patients are doing this:
- Keeping a **symptom journal** with dates, times, and what was happening
- Writing down **who said what**, especially around key decisions or refused tests
- Saving **patient portal messages**, voicemails, and emails
- Taking photos (when appropriate) of visible issues—rash, swelling, surgical site changes
- After an appointment, sending a quick portal message:
> “Just to confirm, today we discussed [X]. The plan is [Y]. I was told [Z].”
Why this goes viral in med mal conversations: when someone says, “The doctor never told me that,” and the record says, “Patient educated, agreed,” patient-side documentation can become a crucial counterweight.
Your medical record tells their version. Your notes tell yours—and together, they create a fuller story if you ever need legal help.
---
5. The “I’m Not Letting This Slide” Right: Complaints, Investigations, and Legal Backup
When something feels seriously wrong—a missed diagnosis, a surgery gone sideways, a medication error—you’re not stuck with just venting online. There are real-world channels with teeth.
Your options may include:
- **Internal hospital complaint systems**: patient relations, quality/safety offices
- **State medical boards** (in the U.S.): they license and discipline doctors
- **Health departments** or regulatory agencies (like CMS in the U.S. for Medicare-covered facilities)
- **Legal consultation** with a medical malpractice attorney
- In some cases, **patient advocates** or ombuds services
Why this matters for your legal rights:
- Complaints and reports create **official records** outside the hospital’s own files.
- Patterns of similar complaints about the same provider can support your case.
- Many med mal lawyers offer **free consultations**—you can find out if what happened rises to the level of malpractice or is “just” bad care.
- There are **deadlines** (statutes of limitations) for filing lawsuits, often a few years or less, sometimes shorter for government-related facilities or children.
Shareable rule of thumb:
> If your gut says, “This feels too big to just move on from,” talk to a lawyer sooner, not later—even if you’re not sure it’s “really” malpractice.
You’re not committing to suing by getting information. You’re making sure time doesn’t silently erase your options.
---
Conclusion
You don’t control everything that happens in a hospital, clinic, or ER. But you’re not a background character in your own medical story.
Your rights to access records, understand your care, get second opinions, document your experience, and push complaints or legal action when necessary are more than legal fine print—they’re built-in tools to protect your health, your safety, and your future.
Share this with the people you love before they end up in a medical crisis. Because the real power move isn’t scrambling for your rights after something breaks—it’s walking into every appointment already knowing where your legal leverage lives.
---
Sources
- [U.S. Department of Health & Human Services – Individuals’ Right under HIPAA to Access Health Information](https://www.hhs.gov/hipaa/for-professionals/privacy/guidance/access/index.html) – Explains your legal right to obtain your medical records and how it works in practice
- [American Medical Association – Informed Consent](https://www.ama-assn.org/delivering-care/ethics/informed-consent) – Outlines ethical and legal standards for informed consent in medical care
- [Agency for Healthcare Research and Quality (AHRQ) – Questions to Ask Your Doctor](https://www.ahrq.gov/questions/index.html) – Provides practical question lists patients can use to understand risks, options, and care plans
- [U.S. Department of Health & Human Services – How to File a Complaint with OCR](https://www.hhs.gov/ocr/complaints/index.html) – Details how to file complaints about privacy, discrimination, and certain health care rights issues
- [Federation of State Medical Boards – Consumer Resources](https://www.fsmb.org/contact-a-state-medical-board/) – Helps patients find and contact their state medical board to check licenses or submit complaints
Key Takeaway
The most important thing to remember from this article is that this information can change how you think about Legal Rights.