You’re hurt, confused, and your gut is screaming, “Something wasn’t right.” But turning that feeling into real legal action? That’s where most people freeze. This is your step‑by‑step, no‑fluff breakdown of what actually happens when you decide to explore a medical malpractice case—plus 5 ultra-shareable power moves people with medical issues are passing around right now.
This isn’t about hating doctors. It’s about protecting yourself when the system glitches and you’re the one paying the price.
---
When “Complications” Might Actually Be Negligence
Not every bad outcome is malpractice—and that’s exactly why the system can feel rigged. Doctors, hospitals, and insurers lean hard on words like “complication,” “rare reaction,” or “unfortunate result.” But legally, the core question is way more specific: did your provider fail to meet the accepted standard of care, and did that failure cause your injury?
Courts don’t compare your doctor to a superhero; they compare them to a reasonably careful provider with similar training in a similar situation. If what happened to you is something another competent doctor would likely have avoided, that’s where negligence lives. And because juries and judges aren’t doctors, the legal process leans heavily on expert witnesses—specialists who explain what should have happened versus what actually did.
This is also why medical malpractice cases are hard, slow, and often expensive. You’re not just proving, “I’m hurt.” You’re proving the how, why, and who messed up, in a way that can survive cross‑examination and insurance-company fire. Understanding this from the start keeps you from being blindsided when a lawyer asks detailed, sometimes uncomfortable questions—even if they’re already on your side.
---
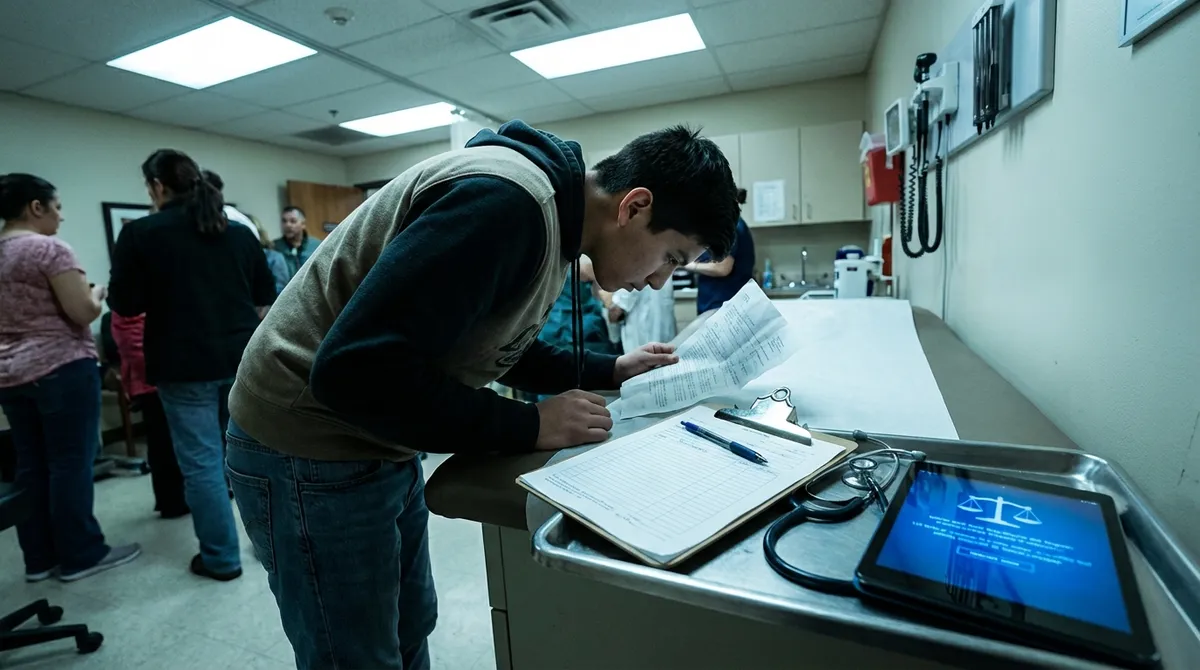
Your Screenshot Era: Building a Legal Story, Not Just a Complaint
Before lawyers file anything, they need a story backed by evidence, not just vibes and anger. That’s where you come in—because you’re the only person who lived every moment of what happened.
Start acting like your own investigator:
- **Request your full medical records** from every provider and facility involved. In the U.S., you have this right under federal law, and they can’t just say no because you might sue.
- Ask for **test results, imaging, medication lists, discharge summaries, and consent forms**—not just the “summary visit notes.”
- Keep a **timeline**: dates, times, who said what, when symptoms changed, when you asked for help and how they responded.
- Track **financial and life fallout**: missed work, extra childcare, rehab costs, mental health impact, travel to appointments.
When you eventually sit down with a lawyer, this turns your situation from “I think something went wrong” into “Here’s a clear chain of events, documented.” That difference can decide whether your case moves forward or stalls at the starting line. You’re not being “dramatic” by documenting; you’re building the backbone of a potential lawsuit.
---
Inside the Legal Machine: What Actually Happens After You Call a Lawyer
From the outside, “I sued” sounds like one big dramatic moment. From the inside, it’s a whole series of quiet, strategic steps. Here’s how the process usually plays out, even if you never see a courtroom:
**Intake + Case Screening**
A med mal attorney (often free consultation) listens to your story and does a quick reality check: is it likely negligence, and are your injuries serious enough to justify a complex case?
**Record Deep Dive + Expert Review**
If it looks promising, the firm gathers your records and sends them to a **medical expert**—sometimes several. Many states won’t even let you **file** the lawsuit unless an expert says your claim is legit.
**Pre-Suit Requirements (State Rules Matter)**
Some states make you send a **notice of intent to sue** or a **certificate of merit** from a medical expert before going to court. Miss these steps and your case can be tossed, even if you’re 100% right on the facts.
**Filing the Lawsuit**
Once filed, the defendant (hospital, doctor, clinic) is officially on the hook to respond. Their insurance company jumps in, and now you’re in the formal legal ring.
**Discovery: The Receipts Phase**
Both sides exchange documents, take depositions (sworn Q&A sessions), and pull in more experts. Discovery is where a lot of cases are **won, lost, or settled**—not at trial.
- **Settlement Talks vs. Trial**
Most med mal cases settle out of court, especially if the defense realizes a jury might be sympathetic. But if the sides can’t agree on who’s responsible and how much your injuries are worth, the case can go to trial—sometimes years after the original injury.
Knowing this structure up front doesn’t make it less emotional. But it does make it less mysterious—and that’s power.
---
5 Viral-Level Legal Power Moves Patients Are Sharing Right Now
These are the “send this to anyone dealing with medical drama” tips that keep blowing up in patient forums and DMs—because they change how you move today, not just “if you ever sue.”
1. Turning “Second Opinions” Into Legal Leverage
A second opinion isn’t just about feeling reassured—it can become key evidence. When you see a new provider:
- Bring your prior records and imaging, but
- Don’t lead with “I’m building a lawsuit.” Just clearly explain what happened, your symptoms, and what you were told.
If the new doctor says your prior care was “concerning,” “outside guidelines,” or “not what I would have done,” those notes may become a powerful piece of your case. Even if you never sue, it helps you get safer, better care going forward.
2. Treating Your Patient Portal Like a Legal Paper Trail
Your online patient portal is quietly one of your best legal receipts:
- Download copies of **messages, test results, and visit summaries** before switching providers or insurance plans.
- Screenshot messaging threads where you reported worsening symptoms, delays, or confusion—and how (or whether) the office responded.
- Save notifications where abnormal results weren’t flagged or explained.
If your care team ignored clear warnings you sent, that’s not just rude—it can be evidence of negligence.
3. Refusing to Be Rushed Through Consent
Informed consent is a legal requirement, not a quick signature for vibes. Before a procedure, you’re supposed to understand:
- The **risks**
- The **benefits**
- The **alternatives** (including “do nothing”)
If you were pressured to sign while sedated, panicked, or barely informed, that can become a serious legal issue later. Start normalizing phrases like:
- “I need more time with this form before I sign.”
- “What happens if we delay this until I understand my options?”
- “Please note in my chart that I asked these questions.”
You’re not “difficult.” You’re documenting that you took consent seriously—even if they didn’t.
4. Knowing Your Deadline: The Clock You Can’t Ignore
Every state has a statute of limitations for medical malpractice—basically a legal expiration date for filing your case. In some places, that deadline can be as short as 1–2 years from when the negligence happened, or when you should reasonably have discovered it.
The catch? Hospitals and insurers know this clock way better than patients do.
If something feels off, don’t wait years hoping it “just gets better” before even talking to a lawyer. A quick legal consult doesn’t mean you’re committing to a lawsuit—it means you’re not accidentally letting your rights expire while you’re still in survival mode.
5. Treating Your Lawyer Like a Strategic Partner, Not a Cleanup Crew
Lawyers can’t magically fix missing records, undocumented conversations, or deadlines that already passed. The earlier you loop in legal help:
- The faster they can **preserve evidence** (like hospital logs, device data, internal notes).
- The better they can coordinate **expert reviews** before memories fade and staff changes.
- The more likely they can help you avoid mistakes—like signing broad releases or lowball settlements with insurers.
Medical malpractice firms often work on contingency fees (they get paid only if you recover money), so it’s not about you cutting a check on day one. Think of them as your system‑translator and strategy team while you focus on healing.
---
Conclusion
When medical care goes wrong, the emotional fallout is massive—but the legal process doesn’t care about feelings; it runs on records, timelines, and expert opinions. That’s why your first moves after something feels off are so critical. Documenting everything, asking sharper questions, grabbing second opinions, and understanding your legal timeline don’t make you “paranoid”—they make you prepared.
You don’t have to become a lawyer to protect yourself. You just have to stop assuming the system will do it for you.
If this hits close to home, don’t keep it in your private group chat. Share it with anyone juggling confusing symptoms, sketchy medical experiences, or that nagging feeling that what happened to them wasn’t “just bad luck.”
---
Sources
- [U.S. Department of Health & Human Services – Individuals’ Right under HIPAA to Access Health Information](https://www.hhs.gov/hipaa/for-professionals/privacy/guidance/access/index.html) - Explains your legal right to obtain copies of your medical records and how providers must respond.
- [American Bar Association – Medical Malpractice Overview](https://www.americanbar.org/groups/public_education/resources/law_issues_for_consumers/medmal/) - Provides a consumer-friendly breakdown of what constitutes medical malpractice and how cases generally work.
- [National Library of Medicine – Informed Consent in Healthcare](https://www.ncbi.nlm.nih.gov/books/NBK430827/) - Details the legal and ethical standards for informed consent and why it matters in malpractice cases.
- [Cornell Law School Legal Information Institute – Statute of Limitations](https://www.law.cornell.edu/wex/statute_of_limitations) - Explains what statutes of limitations are and why timing is critical in civil cases like medical malpractice.
- [Agency for Healthcare Research and Quality – Patient Safety Primer: Medical Errors and Adverse Events](https://psnet.ahrq.gov/primer/medical-errors-and-adverse-events) - Discusses how medical errors happen and how they’re identified, providing context for potential malpractice situations.
Key Takeaway
The most important thing to remember from this article is that this information can change how you think about Legal Process.