You shouldn’t have to become a mini-doctor and a mini-lawyer just to stay safe in the healthcare system—but here we are. The good news? A few smart, repeatable habits can lower your risk of medical errors and make you legally ready if something goes sideways. Think of this as your “IRL health filter”: it doesn’t replace doctors, but it seriously cleans up the chaos.
Below are five ultra-shareable prevention moves people with chronic issues, new diagnoses, or just too many appointments will actually use—and want to send to their group chat.
---
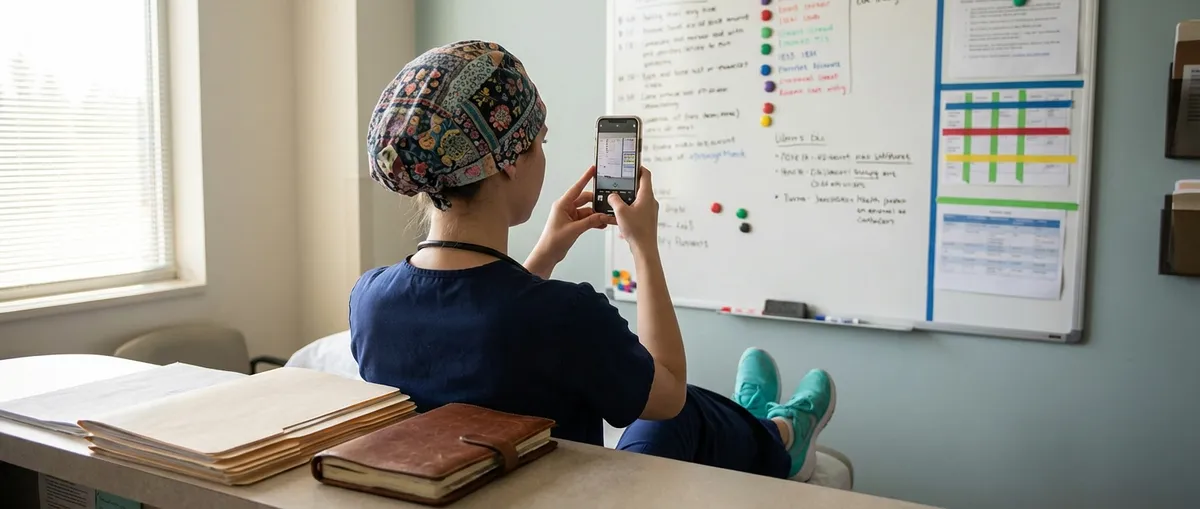
1. Turn Every Appointment Into a Screenshot Session
If your medical life isn’t documented, it basically lives on “airplane mode.”
Make it normal to “screenshot your health” in real time. That means:
- Snapping photos (where allowed) of medication labels, discharge papers, and after-visit summaries
- Taking a quick pic of the whiteboard in your hospital room (names of staff, daily plan, goals)
- Saving screenshots of test results and messages from patient portals
- Using your notes app to jot down what the doctor said—*while they’re talking*
Why this prevents med mal: when you can see the timeline—what meds were changed when, what instructions you were given, who said what—it’s easier to catch dangerous mix-ups early. For example, if your new prescription contradicts last month’s cardiology instructions, your screenshots make that clash obvious.
Bonus: if things ever do go legally sideways, organized screenshots and time-stamped notes are digital gold.
---
2. Run the “Explain It Like I’m Sending This to My Mom” Test
If you can’t explain your diagnosis or treatment to someone else in plain language, you don’t understand it well enough—and that’s a risk.
Before you leave the appointment, ask your provider to break it down so clearly that you’d feel confident texting it to your mom or best friend. Try lines like:
- “Can you walk me through this like I’m brand new to medicine?”
- “What exactly is wrong, what are we doing about it, and what happens if we don’t?”
- “If I had to explain this plan in two sentences, what should I say?”
Then repeat it back:
“So I have ___, we’re doing ___, and I should watch for ___, right?”
This “teach-back” moment is huge. Research shows that when patients repeat instructions back, errors and readmissions drop. It also flushes out misunderstandings on the spot instead of three days later at 2 a.m. when your symptoms flare and your panic spikes.
Health understanding isn’t just “nice to have”—it’s a frontline defense against wrong meds, missed follow-ups, and preventable emergencies.
---
3. Build a “Medical Hype Squad” Chat Before You Actually Need It
If you’re handling health stuff alone, you’re more vulnerable to bad communication, missed red flags, and rushed decisions.
Create a tiny “Med Squad” group chat now—before things get serious. Add:
- One practical friend or family member who asks sharp questions
- One calm person who steadies you when you’re spiraling
- Optional: a health-nerd friend who loves reading articles and studies
Use the chat to:
- Drop appointment summaries (“Doctor said it’s probably X, ordered Y test.”)
- Share pics of instructions/med lists for a second pair of eyes
- Crowdsource questions to ask at your next visit
- Ask someone to come as your real-life backup for surgeries or big decisions
Why this prevents med mal: when you’re stressed or in pain, your brain is not in note-taking mode. A hype squad helps you catch “wait, that doesn’t match what they told you last time” moments. Extra brains = fewer mistakes slipping through.
And if something feels off, you’ve already got an instant support team ready to say, “Nope, get a second opinion.”
---
4. Treat Every New Med Like a Collab That Needs a Fact-Check
Medication errors are one of the most common medical mistakes, and they’re often preventable if patients double-check what they’re given.
Whenever you’re prescribed something new—or your dose changes—run a quick, repeatable med safety script:
Ask your provider or pharmacist:
- What is this drug *for* in my specific case?
- What’s the exact name, dose, and how often do I take it?
- How long should I be on it?
- What are the top *3* side effects I should actually watch for, not the whole scary list?
- Does this clash with anything I’m already taking (including vitamins, herbal stuff, or OTC meds)?
Then cross-check:
- Compare the bottle label with what your doctor said (name, dose, timing)
- If it looks different from what you had before, ask *why*
- Use a reputable site (like Mayo Clinic or MedlinePlus) to read a quick overview—just enough to know if something sounds off
This isn’t about “Dr. Google vs. my doctor.” It’s about making sure your treatment plan isn’t relying on everyone having a perfect day with zero typos, zero mix-ups, and zero misclicks in the electronic chart.
You’re not being “difficult.” You’re being the last safety check in the system that’s supposed to protect you.
---
5. Screenshot Your Symptoms Like You’re Building a Case (Because You Are)
Most medical errors don’t show up as one big dramatic moment—they show up as a pattern no one connected in time.
Turn your symptoms into a running, organized story:
- Use a notes app or symptom tracker to log:
- What you felt
- When it started (date + time)
- What you were doing
- What made it better or worse
- Any meds you took around then
- Take photos or short videos of visible symptoms (rashes, swelling, breathing difficulty you can hear, tremors, etc.)
- Add “pain score” (0–10) and how it affects daily life (“couldn’t drive,” “missed work,” “woke up all night”)
Why this prevents med mal: strong, specific symptom history helps your provider spot red flags early—like signs of infection, dangerous drug reactions, or conditions your first visit might have missed. It also makes it harder for anyone to say “It didn’t seem that bad” when your tracked reality says otherwise.
If you ever do need legal backup, this kind of documented pattern is the difference between “I think it was getting worse” and “Here’s exactly how it escalated, with timestamps.”
---
Conclusion
You shouldn’t need a law degree and a medical degree just to get safe, decent care—but building a few “clinic-ready, lawyer-smart” habits gives you serious leverage in a messy system.
- Screenshot what matters
- Make doctors explain things in textable language
- Build a tiny hype squad around your health
- Treat every new med like a partnership, not a blind trust
- Track your symptoms like the story they are
None of this makes you “difficult.” It makes you the one person in the room who’s 100% invested in your outcome: you.
Share this with the person in your life who’s always at an appointment, always on hold with a clinic, or always saying, “Something just doesn’t feel right.” These are the quiet moves that prevent medical mistakes—and, when needed, power up a future med mal case.
---
Sources
- [Agency for Healthcare Research and Quality (AHRQ): 20 Tips to Help Prevent Medical Errors](https://www.ahrq.gov/patients-consumers/care-planning/errors/20tips/index.html) - Federal patient safety guidance on how patients can reduce their risk of medical errors
- [Centers for Disease Control and Prevention (CDC): Patient Engagement](https://www.cdc.gov/antibiotic-use/patients/index.html) - Practical tips on talking with clinicians and using medications safely
- [Mayo Clinic: Patient Safety – What You Can Do to Be a Safe Patient](https://www.mayoclinic.org/patient-visitor-guide/preparing-for-your-visit/patient-safety) - Strategies patients can use before, during, and after appointments to stay safe
- [MedlinePlus: Talking With Your Doctor](https://medlineplus.gov/talkingwithyourdoctor.html) - NIH-backed resource on asking questions, understanding instructions, and preventing misunderstandings
- [National Academy of Medicine: Improving Diagnosis in Health Care](https://nam.edu/improving-diagnosis-in-health-care/) - Explains how diagnostic errors happen and why patient participation is critical in preventing them
Key Takeaway
The most important thing to remember from this article is that this information can change how you think about Prevention Tips.