You don’t need a med degree to protect yourself from medical mistakes—you need strategy. In a system that’s rushed, understaffed, and sometimes dismissive, the most powerful safety tool in the room is you paying attention and backing it up with receipts.
This isn’t about fighting your doctor. It’s about turning every appointment, test, and prescription into a protected zone where your health—and your rights—come first. Share this with anyone who’s ever walked out of an appointment thinking, “Wait… did that feel off?”
---
1. Turn Every Appointment Into a “Shared Notes” Meeting
If your medical visit isn’t a two-way conversation, it’s a risk zone.
Walk in like you’re co-running the appointment:
- Open your Notes app and title it with the date + doctor’s name.
- As they talk, repeat back key points: “Just to confirm—this medication is for X, I take it Y times a day, and the side effects I should watch for are Z, right?”
- If they rush, pause them: “I need to write this down. Please say that again.”
- Before you leave, say: “Can you summarize today’s plan in 30 seconds so I make sure I got it right?”
Why this blocks problems:
When instructions are vague or misunderstood, errors happen—wrong doses, missed follow-ups, delayed diagnoses. Verbal “clarification” + your written recap creates a real-time safety net. It also quietly builds a timeline that matters a lot if something later goes wrong.
Bonus power move: Ask if your clinic uses an online portal (like MyChart). Check visit summaries and messages regularly and screenshot anything important. If something doesn’t match what you were told, ask for it to be corrected in writing.
---
2. Make Second Opinions Your Default, Not Your Drama
A second opinion is not betrayal. It’s basic quality control in a complicated system.
Use this any time you feel:
- Brushed off (“It’s just stress” with no testing)
- Rushed into surgery or major procedures
- Confused by a diagnosis that doesn’t match your symptoms
- Like no one is connecting the dots between multiple issues
- “This is a lot to process. I’d like another specialist to review this before I decide.”
- “Are there alternative treatments another doctor might suggest?”
- “Can you recommend someone for a second opinion who sees a lot of cases like mine?”
How to ask without awkward vibes:
Why this blocks medical malpractice:
Misdiagnosis and delayed diagnosis are massive drivers of malpractice claims. A fresh set of eyes can catch what the first person missed. It’s not “being difficult”—it’s standard practice in complex medicine.
If a provider shames you for asking or refuses to share records promptly? That’s not just a red flag—that’s a klaxon. Save every message, email, and note from that point on.
---
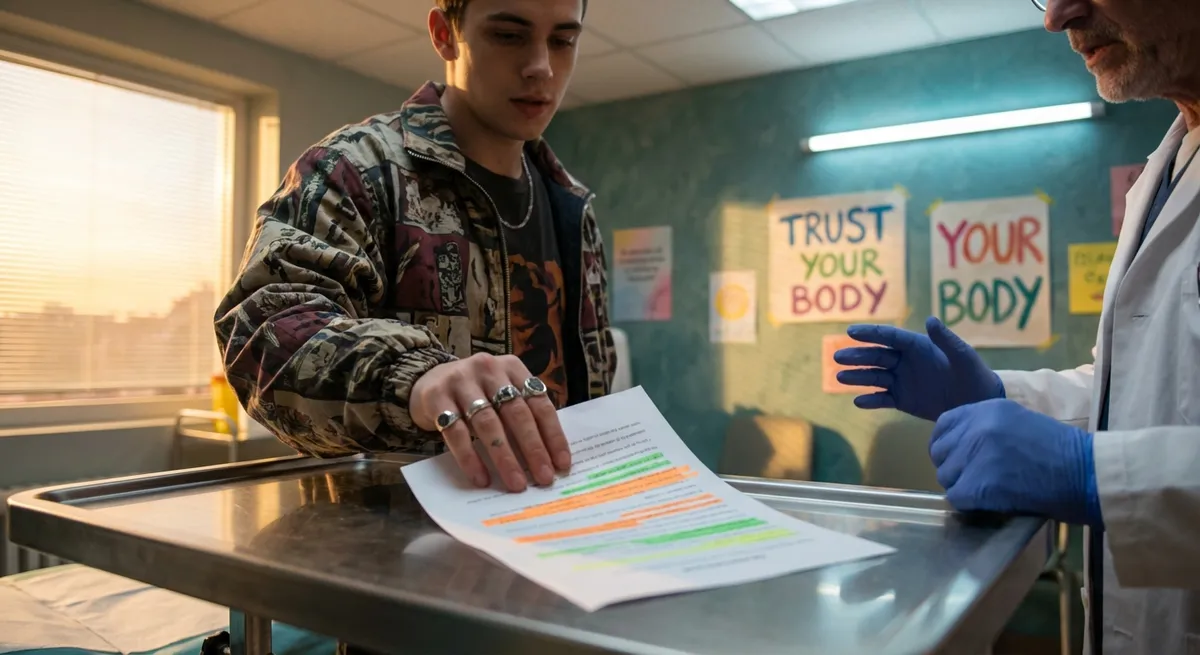
3. Treat Consent Forms Like Contracts, Not Stickers You Sign on the Way In
That clipboard (or tablet) before a procedure? It’s not just paperwork—it’s the legal backbone of what they’re allowed to do to your body.
Here’s how to flip from passive signing to active protecting:
- Don’t sign until someone *talks you through* the form in plain language.
- Ask: “What are the top 3 risks you’re most worried about for *me* specifically?”
- Ask: “What are my realistic options if I say no or want to wait?”
- If the form is vague (or just says “I understand the risks”), say:
“Please document the specific risks we discussed in the record and that we talked about alternatives.”
Why this matters legally and medically:
Informed consent isn’t just a buzz phrase—it’s a legal requirement. If you weren’t clearly told about risks, alternatives, or what happens if you choose nothing, that can be central in a med mal case. More importantly, it helps you catch rushed or unsafe recommendations before they happen.
If anything feels off, you can say: “I’m not comfortable signing this today. I’d like more time to think and ask questions.” You are allowed to leave. You are allowed to change your mind.
---
4. Sync Your “Real Life” Story With Your Medical Record Story
Medical mistakes love one thing: missing context.
Doctors often see you in tiny slices—10 minutes here, a lab result there. But your life is 24/7. When your lived reality and your chart don’t match, wrong assumptions get made, and that can spiral fast.
Protect yourself by syncing your story:
- Bring a one-page “health snapshot”: major diagnoses, meds, allergies, surgeries, and any big changes in symptoms.
- Any time your story changes (“I’m way more tired than usual,” “This pain is now daily, not weekly”), say:
- If a provider says, “Your labs are normal,” ask:
“Please add this to my chart exactly as I’m describing it. This is new and different for me.”
“Can you show me? What exactly are the numbers, and what range are you using?”
Why this stops problems early:
Charts with missing or outdated info fuel wrong diagnoses, unsafe medications, and missed emergencies. Getting your actual reality written down creates a paper trail that shows you were flagging a problem—even if someone initially ignored it.
Hot tip: At least once a year, request copies of your records or download them from your portal. If something big is wrong (like allergies missing or incorrect conditions listed), ask in writing for corrections. That’s a quiet but powerful prevention move.
---
5. Build a “Medical Backup Squad” Before You Ever Need a Lawyer
Your future self will thank you for this one.
Don’t wait until something goes really wrong to start building your support system. Prevention includes knowing exactly who you’ll call and what you’ll pull up if care goes sideways.
Your low-key safety kit:
- A shared folder (Google Drive, iCloud, etc.) with: test results, hospital discharge papers, medication lists, and key messages.
- One trusted person who knows where everything is and can step in if you’re out of it.
- Your state’s medical board website bookmarked so you can quickly check a doctor’s license and discipline history.
- A short note on your phone called “If Something Goes Wrong” with:
- Your main doctors
- Allergies
- Current meds
- Emergency contact
- Any major past complications from treatment
Why this is a big deal:
If there is negligence—a missed diagnosis, a botched procedure, a dangerous medication interaction—the people who can help you (new doctors, patient advocates, and yes, medical malpractice attorneys) will move much faster if your receipts are organized.
And here’s the twist: the same receipts that make a strong legal case also tend to reveal problems earlier—so you can switch providers or demand better care before things escalate.
---
Conclusion
You are not “overreacting” when you ask questions, take notes, or slow things down. You’re doing what the safest, most empowered patients do: turning your medical life into something documented, double-checked, and shared—not just blindly trusted.
Medical malpractice isn’t just about what happens in the operating room. It’s the rushed visit where no one listens, the diagnosis that never gets verified, the consent form you sign half-confused and half-pressured.
When you:
- Co-run your appointments
- Normalize second opinions
- Treat consent like a real conversation
- Sync your lived reality with your chart
- And build that medical backup squad
…you’re not just “being careful.” You’re actively lowering your risk of preventable harm—and quietly building legal and medical protection if something still goes wrong.
Share this with the people you love. One screenshot at the right moment can change how someone handles the most important appointment of their life.
---
Sources
- [Agency for Healthcare Research and Quality – Questions to Ask Your Doctor](https://www.ahrq.gov/questions/resources/index.html) – Practical guidance on what to ask during visits to improve safety and understanding
- [Centers for Disease Control and Prevention – Patient Engagement](https://www.cdc.gov/patient-safety/patients.html) – Explains how active patient participation helps prevent medical errors and complications
- [American Medical Association – Informed Consent](https://code-medical-ethics.ama-assn.org/ethics-opinions/informed-consent) – Outlines ethical and legal standards for informed consent in medical care
- [Johns Hopkins Medicine – Medical Errors and Patient Safety](https://www.hopkinsmedicine.org/patient-safety) – Discusses how and why errors happen and what patients can do to stay safer
- [National Library of Medicine (NIH) – Diagnostic Errors in Medicine](https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3120548/) – Research article explaining how misdiagnosis occurs and the impact on patient outcomes
Key Takeaway
The most important thing to remember from this article is that this information can change how you think about Prevention Tips.